Overview:
Indicated in cases with total loss of buccal wall in combination with thin periodontal biotype or gingival recession. IDR II Protocol will explain how to manage compromised sockets with low or no remaining bone in combination with immediate implant placement, bone reconstruction and provisional fabrication in a single procedure using a combination of bone and soft tissue graft harvested from maxillary tuberosity.
• EXTRACT DAMAGED TOOTH AND REMOVE GRANULATION TISSUE AND REMAINS OF PERIODONTAL TISSUE.
• USE THE DENSAH® BURS IN OD MODE (CCW ROTATION) TO PREPARE THE IMPLANT SITE AND DENSIFY THE BONE BED.
• ANCHOR THE IMPLANT INTO THE PALATAL WALL.
• HARVEST THE TRIPLE GRAFT AND FILL THE GAP.
• PLACE A MANUFACTURED SCREW RETAINED PROVISIONAL RESTORATION WITH AN ADEQUATE EMERGENCE PROFILE (CEMENTED RESTORATION MUST NOT BE UTILIZED).
• ALLOW A MINIMUM 4 MONTHS HEALING AND PLACE A SCREW RETAINED FINAL PORCELAIN CROWN
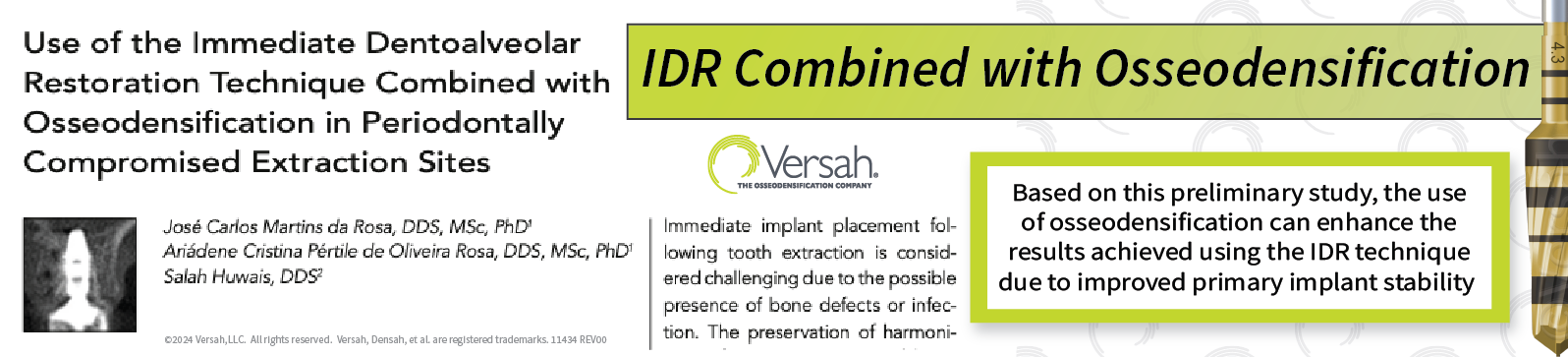
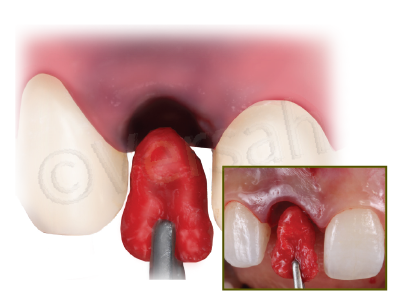
Step 1:
Extract the damaged tooth using a minimally invasive procedure to preserve the remaining bone. Completely remove the granulation tissue and the remains of periodontal tissue or any granulation tissue by carefully using the curettage technique in the socket. Total loss of the buccal wall might be common and evident.
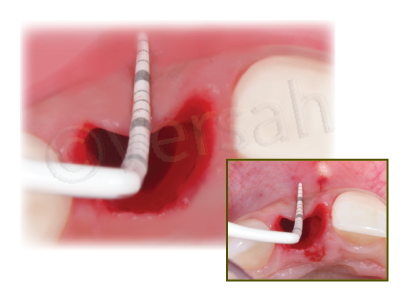
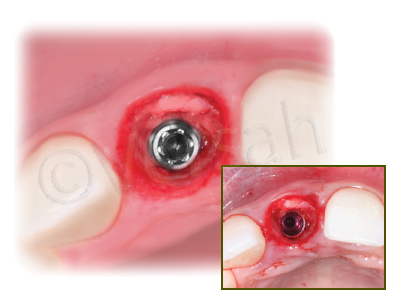
Step 2:
Use the Densah® Burs to prepare the implant site. Start with the Densah® pilot drill, in clockwise mode, to a depth related to the planned implant length. Depending upon the implant type and diameter, follow with wider Densah® Burs corresponding with the Implant System Drilling Protocol.* Starting with the smallest Densah® Bur, run the Densah® Burs in OD mode (counterclockwise, with speed 800-1500 rpm with copious irrigation).
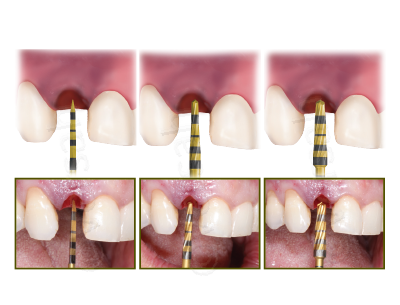
Step 3:
Anchor the implant into the remaining palatal bone in the 3-D position.
Step 4:
Harvest the triple graft (connective tissue, cortical and cancellous bone in one single piece) from the maxillary tuberosity. Insert the triple graft into the buccal defect aspect of the receptor site to recover hard and soft tissue that is lost.
Step 5:
Compact particulate autogenous bone harvested from the maxillary tuberosity to fully fill the gap around the implant, especially in the buccal aspect.
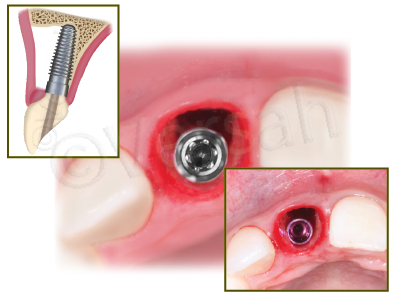
Step 6:
Place a manufactured screw retained provisional restoration with an adequate emergence profile.

Step 7:
Allow a minimum 4 months of healing for soft tissue to become stable in volume and have adequate thickness. A screw retained final restoration is recommended. Maintenance of the anatomical contour of soft tissue can be observed.


Clinical follow-up showing stability of soft tissue regarding gingival margin and papillae.
A CBCT image after 4 years highlights the stability of the buccal wall, in terms of thickness and height.
Case courtesy of Dr. José Carlos da Rosa
* Data on file, versah.com/our-science/ for studies
Clinician judgement and experience should be applied in conjunction with this clinical practice suggestive use protocol.
10523 REV03 03/2024