Overview
Osseodensification will not create the tissue, it may only optimize and preserve what already exists. There is a need for ≥ 2 mm of trabecular-bone core and ≥ 1/1 trabecular/cortical bone ratio to achieve a predictable plastic expansion. The more cortical bone there is, the more trabecular core is needed to facilitate predictable expansion. The ideal minimum ridge to expand is 4 mm (2 mm trabecular core + 1mm cortex on each side). This protocol is indicated to expand a ridge with a narrow crest and wider bas It is not indicated in resorbed ridge with a narrow base.
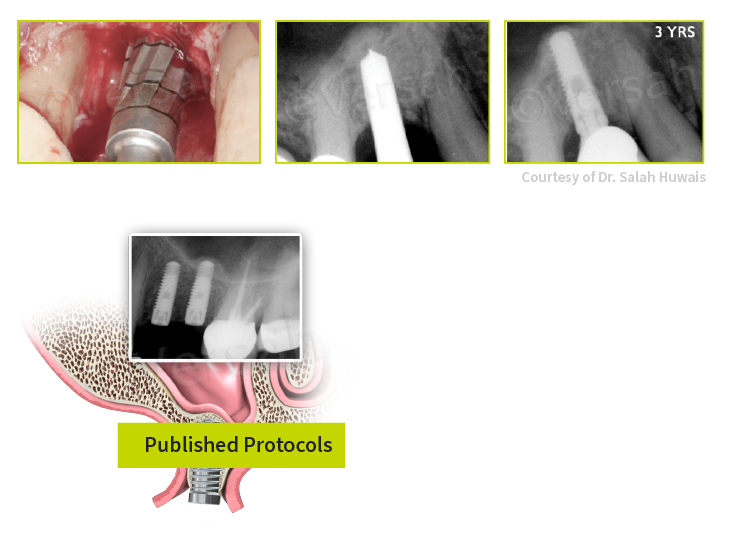
Overview
Minimum residual bone height ≥ 6mm.
Use Densah® Burs in full step increments. For example: 2.0, 3.0, 4.0, 5.0 mm.
Measure bone height to sinus floor.
Take pilot drill to 1 mm below the sinus floor.
Densah® Bur (2.0) in OD mode (CCW) to sinus floor.
Enter the sinus with Densah® Bur (3.0) in OD mode (CCW) in 1 mm increments to a maximum level of 3 mm past the sinus floor.
Densah® Bur (4.0), (5.0) in OD mode (CCW) to maximum level of 3 mm past the sinus floor if needed.
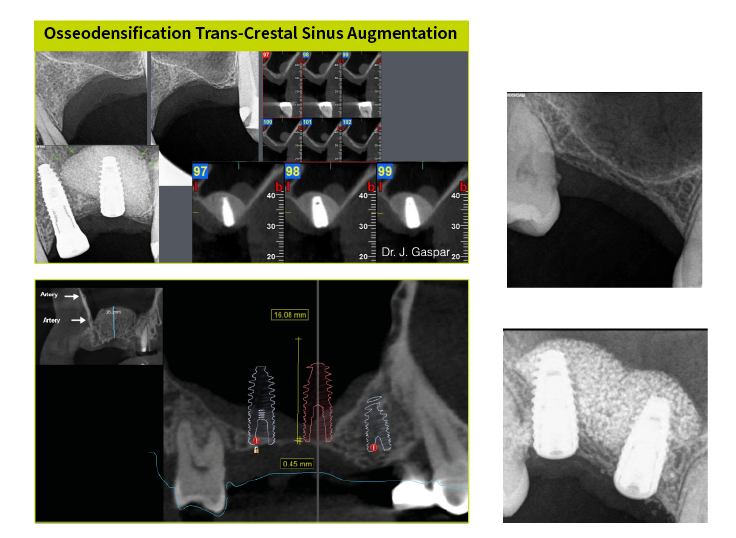
Overview
Minimum residual bone height 4-5 mm.Use Densah® Burs in full step increments. For example: 2.0, 3.0, 4.0, 5.0 mm.
Measure bone height to sinus floor.
Take Densah® Bur (2.0) in OD mode (CCW) to sinus floor.
Enter the sinus with Densah® Bur (3.0) in OD mode (CCW) in 1 mm increments to a maximum level of 3 mm past the sinus floor.
Densah® Bur (4.0), (5.0) in OD mode (CCW) up to 3 mm past the sinus floor if needed.
Use the last Densah® Bur in low speed with no irrigation to gently propel well hydrated allograft.
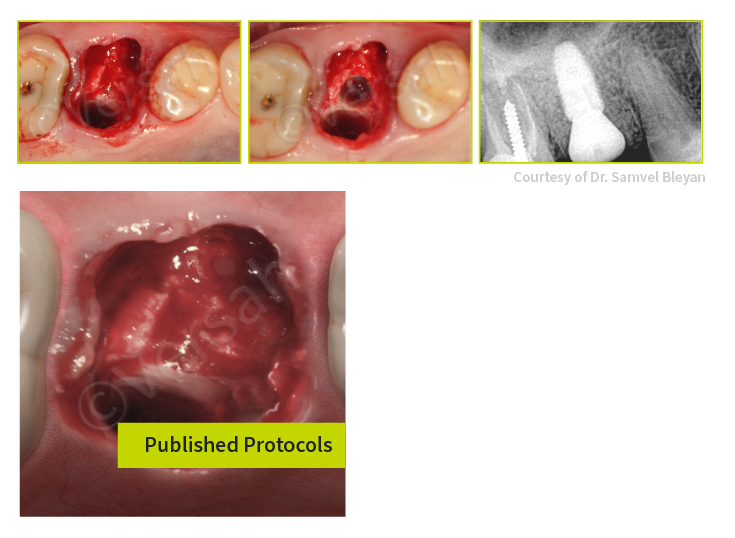
Overview
Implant Stability must be mainly provided by the apical portion of the socket.
Atraumatic tooth extraction with no or minimal flap reflection.
Implant diameter to be slightly wider than the tooth apex.
Final Densah® Bur diameter to be ≥ apical diameter of the apex.
Use a well hydrated allograft (cancellous/cortical) to fill the socket.
Use Densah® Bur that is one step smaller than the last one used to prepare the osteotomy, to compact the allograft.
Implant stability must be mainly achieved by the apical portion of the extraction socket.
Overview
Separate molar roots at the furcation without compromising the integrity of the septum. Implant placement should be either at the crest or sub-crest level. Fill the gap with a bone graft material if needed; preferably an allograft with a 70/30 cancellous/cortical ratio.
Overview
Indicated for upper molar sites with a minimum of 4mm wide septum. Utilize CBCT imaging to measure ridge width and distance to the sinus floor.
Flapless atraumatic tooth extraction with minimum trauma to preserve septum.
Osseodensification instrumentation using Densah® Burs in CCW (800–1500 rpm) to expand the septum and lift the sinus membrane simultaneously.
Implant Placement. Graft the socket around the implant with the appropriate bone graft materials.
Seal the socket with a large/wide healing abutment.
Overview
For cases with initial ridge width of < 3.0 mm. Graft the newly formed socket with a 70/30 cancellous/cortical combination allograft. Allow healing for 3–6 months, then re-enter the site to prepare for implant placement using Osseodensification with the Densah® Burs.
Overview
The Versah® C-Guide® Guided surgery is an innovative system that allows for adequate irrigation, proper visualization of the osteotomy expansion/preparation, freedom to luxate the Densah Bur®, and the ability to manage multiple sites with different preparation depths and diameters with precision.
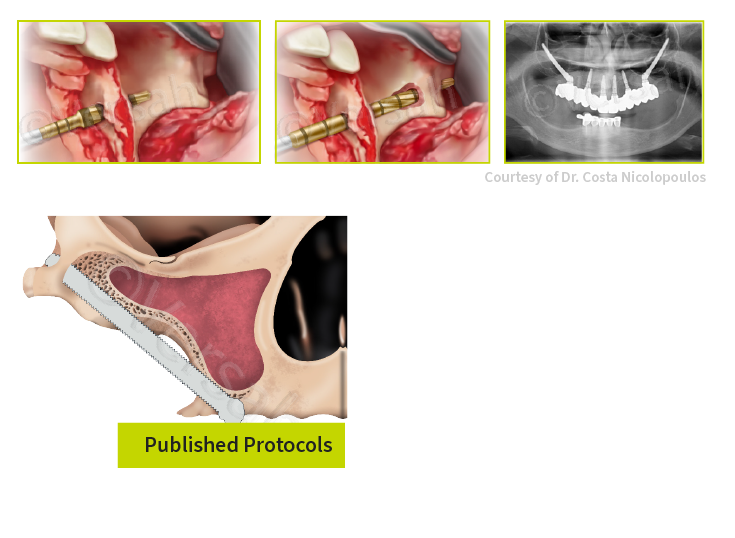
Overview
The anterior maxillary wall is slightly more concave. The pathway is totally intra-maxillary with an intra/extra-sinus approach. A tunnel osteotomy is created through the alveolar crest, into the sinus internal lateral wall, to slightly come out through that lateral wall and then re-enter again as a second tunnel osteotomy into the sinus to come out through the body of the zygoma.
Overview
In these cases, the anterior maxillary wall is very concave. The pathway is intra-maxillary with a totally extra sinus path. A tunnel osteotomy is created through the alveolar crest to come out into the external maxillary wall and then re-enter again as a second tunnel osteotomy into the body of the zygoma to come out through the superolateral aspect of the body of the zygoma. Between the two tunnel osteotomies the maxillary wall is very concave and therefore, there is no groove/channel osteotomy between them — i.e., the middle part of the implant body would not touch the most concave part of the wall.
Overview
This ZGO protocol IV follows an extra-maxillary path. The maxilla and alveolar bone show extreme vertical and horizontal atrophy. The pathway is extra-maxillary with a totally extra sinus path. The implant head is located buccal to the alveolar crest, usually in a shallow “channel” osteotomy. Most of the zygomatic implant body has an extra sinus/extra-maxillary path. The coronal part of the zygomatic implant is extra-maxillary, usually in a “channel” osteotomy, whereas the apical part of the implant is surrounded by bone in a “tunnel” osteotomy in the zygomatic bone. The zygomatic implant contacts bone in the zygomatic bone and part of the external lateral sinus wall.
Overview
Indicated in cases with poor-quality soft tissue due to fracture and infection in post-extraction sockets in combination with severe bone loss. IDR I Protocol introduces a new perspective to manage these compromised sockets using flapless surgery in a simple way based on biological response.
Overview
Indicated in cases with total loss of buccal wall in combination with thin periodontal biotype or gingival recession. IDR II Protocol explains how to manage compromised sockets with low or no remaining bone in combination with immediate implant placement, bone reconstruction, and provisional fabrication in a single procedure using a combination of bone and soft tissue graft harvested from the maxillary tuberosity.
Overview
Indicated in cases of non-restorable anterior and posterior teeth indicated for Socket Shield procedure.
Data on file, versah.com/our-science/ for published studies
** Clinician judgement and experience should be applied in conjunction with this clinical practice suggestive use protocol